EMSOW Weekly Newsletter – January 15, 2020
Posted on January 15, 2020
[#19412] Do not create patient statements for claims forwarded to a secondary payer
We have updated our payment posting feature to prevent errors and improve your billing accuracy. From now on, the system will not create a patient statement when you are posting a payment from an ERA that indicates that the original claim was forwarded to a secondary insurance carrier. If the secondary insurance is not entered into the service record, an error message will be displayed, asking the user to add the secondary insurance to the service.
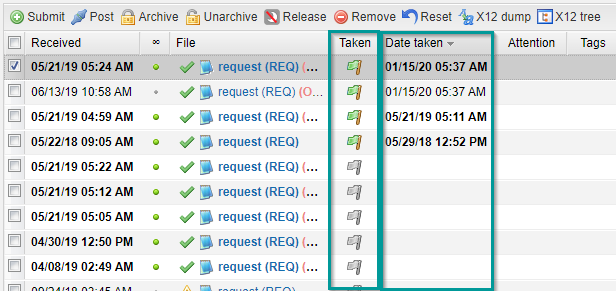
[#19372] Updates in the Clearing module
To further improve your billing accuracy, we have also updated the Clearing module. Now, before you mark a file as taken by ticking the flag icon in the Taken column, you will see a confirmation window. To mark the file as taken, click Yes. Besides, we have added the Date taken column so that you could easily track the date and time of when the files were taken.
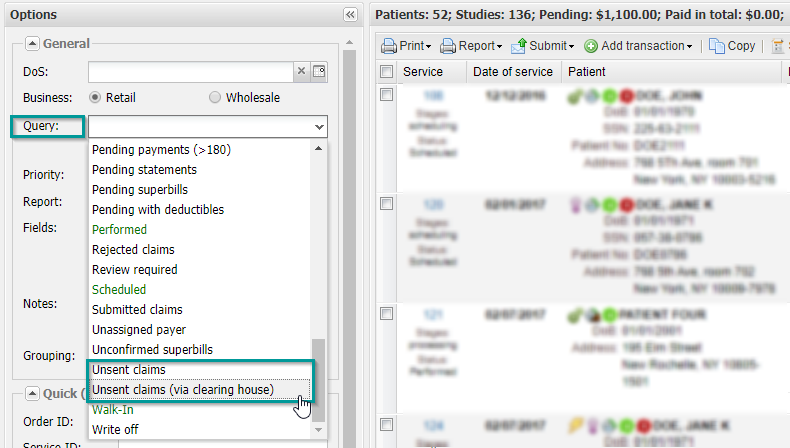
[#19482] Improved claims search
Now you can gain better control over your revenue streams. Previously, the Unsent claims filter disregarded the claims that users marked as submitted manually, so the filter would display those claims as if they were unsent. We have fixed this issue. Also, we have added a new filter, Unsent claims (via clearing house), which allows you to search specifically for claims that are supposed to be sent electronically.
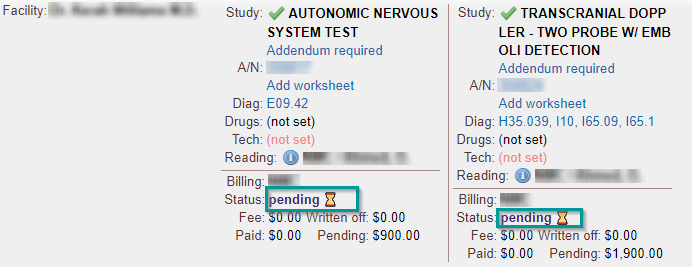
[#19490] Billing status icons in the Processing module
You asked us to visualize the billing status of exams in the Processing module, and we did it. We have added visual icons to the billing status line. Now, along with the textual description, you will see status icons: ✅ for paid exams, ⌛ for pending payments, and ✍️ for written-off amounts. This update will help your staff see the billing status of the exams at a glance!